Novel agent works against resistant TB
The investigational drug delamanid may help combat multidrug-resistant tuberculosis, results of a phase II trial indicate.
When added to background therapy with second-line agents for 2 months, two different doses of delamanid resulted in higher rates of sputum-culture conversion than placebo, according to Lawrence Geiter, PhD, of Otsuka Pharmaceutical in Rockville, Md. -- which is developing the agent -- and colleagues.
That endpoint has been associated with improved clinical outcomes among patients infected with strains of Mycobacterium tuberculosis that are resistant to the first-line agents isoniazid and rifampin, the researchers reported in the June 7 issue of the New England Journal of Medicine.
Effective treatment for multidrug-resistant tuberculosis is an unmet need, Richard Chaisson, MD, and Eric Nuermberger, MD, of Johns Hopkins, wrote in an accompanying editorial. They added, however, that the current study -- like others of novel tuberculosis drugs -- does not help clinicians identify the most effective combinations of medications.
"It is important to accelerate research to identify the best regimens of new and existing drugs and guide clinicians in the most effective application of these drugs," they wrote. "Regulatory agencies should consider this imperative in their guidance to prospective sponsors and in their review of applications for the registration of new agents."
Each year, there are about 440,000 cases of multidrug-resistant tuberculosis around the world, accounting for about 5% of all tuberculosis cases.
Another study in the same issue of NEJM by Yu Wang, MD, of the Chinese Center for Disease Control in Beijing, and colleagues highlighted the problem in China. In a survey, the researchers found that among newly diagnosed patients, 34.2% had some form of drug resistance, 5.7% had multidrug resistance, and 0.5% had extensive resistance.
The rates were even higher among previously treated patients, which Chaisson and Nuermberger attributed to poor management of the initial cases, breeding more resistance.
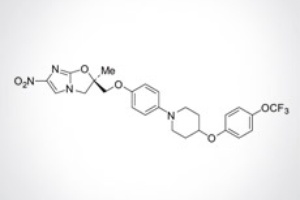
Geiter and colleagues evaluated the use of delamanid, a nitro-dihydro-imidazooxazole derivative that inhibits mycolic acid synthesis, for the treatment of multidrug-resistant disease. The agent previously showed activity against drug-resistant strains in preclinical studies.
Their phase II trial included 481 patients ages 18 to 64 (median 35), 68.4% of whom were male with pulmonary multidrug-resistant tuberculosis recruited at 17 centers in nine countries -- the Philippines, Peru, Latvia, Estonia, China, Japan, Korea, Egypt, and the U.S.. Only four patients had HIV.
Each patient was randomized to one of three groups:
- Delamanid 100 mg twice daily
- Delamanid 200 mg twice daily
- Placebo twice daily
Treatment lasted for 2 months and was given on a background regimen consistent with World Health Organization guidelines. That generally included four or five anti-tuberculosis medications, including any first-line medications to which the patient's disease remained susceptible, an injectable anti-tuberculosis medication (an aminoglycoside or capreomycin), a fluoroquinolone, and other drugs.
The primary efficacy endpoint was the percentage of patients with sputum-culture conversion in a liquid broth medium at 2 months. Conversion was defined as a series of at least five weekly cultures that were negative for growth of the bacteria.
The rate of conversion was 45.4% with the lower dose of delamanid, 41.9% with the higher dose, and 29.6% with placebo. The differences between both drug groups and the placebo group were statistically significant at P<0.05.
"No dose-response effect was observed, and the margin of benefit was significant but modest," wrote Chaisson and Nuermberger in their editorial. "Nonetheless, increased sputum-culture conversion rates of this magnitude are historically associated with a reduction in the duration of treatment needed to cure tuberculosis."
Most of the adverse events observed during the study were mild or moderate in severity, and the rate did not differ between the three groups. Overall, 2.9% of patients stopped treatment because of adverse events.
The most common adverse events were gastrointestinal, including nausea (36% with the lower dose, 40.6% with the higher dose, and 33.1% with placebo), vomiting (29.8%, 36.2%, and 27.5%), and upper abdominal pain (25.5%, 22.5%, and 23.8%).
The rate of QT prolongation was higher in the delamanid groups -- 13.1% with the higher dose and 9.9% with the lower dose -- than in the placebo group (3.8%). There were, however, no clinical events -- including syncope or arrhythmias -- associated with the issue.
Chaisson and Nuermberger said the drug has an acceptable adverse event profile, although cardiotoxicity is a potential concern.
The delamanid study was funded by Otsuka Pharmaceutical Development and Commercialization, which provided the study drug. Company employees designed the study with input from an academic author and wrote the manuscript. Geiter and one of his co-authors are paid employees of Otsuka Pharmaceutical Development and Commercialization. The other authors reported relationships with Otsuka, Kendle International, Documed, the North Estonia Medical Foundation, and the State Agency "Infectology Center of Latvia" Clinic of Tuberculosis and Lung Diseases.
The study by Wang and colleagues was funded by the Chinese Ministry of Health. The authors reported that they had no conflicts of interest.
Chaisson reported receiving grants or having grants pending from the NIH and CDC for tuberculosis studies. His wife is a stockholder of Merck. Nuermberger has received research grants from Otsuka, Pfizer, and the Global Alliance for TB Drug Development. He has a patent pending through his institution for "Combination therapy of tuberculosis."
Primary source: New England Journal of Medicine
Source reference:
Gler M, et al "Delamanid for multidrug-resistant pulmonary tuberculosis" N Engl J Med 2012; 366: 2151-2160.
Additional source: New England Journal of Medicine
Source reference:
Chaisson R, Nuermberger E "Confronting multidrug-resistant tuberculosis" N Engl J Med 2012; 366: 2223-2224.
Additional source: New England Journal of Medicine
Source reference:
Zhao Y, et al "National survey of drug-resistant tuberculosis in China" N Engl J Med 2012; 366: 2161-2170.
MedPage Today
http://www.medpagetoday.com/InfectiousDisease/Tuberculosis/33116